Volume 11, Issue 2 (Summer 2024)
J Prevent Med 2024, 11(2): 152-161 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fakhri S, Yazdan Panah A, Aghaee Borzabad P. The Challenges in the Implementation of the Family Physician Program in Minab City, Hormozgan Province, South of Iran. J Prevent Med 2024; 11 (2) :152-161
URL: http://jpm.hums.ac.ir/article-1-778-en.html
URL: http://jpm.hums.ac.ir/article-1-778-en.html
1- Department of Health and Medical Services Management, Faculty of Humanities, Marvasht Branch, Islamic Azad University, Marvasht, Iran.
2- Determinants of Health Research Center, Yasuj University of Medical Science, Yasuj, Iran.
2- Determinants of Health Research Center, Yasuj University of Medical Science, Yasuj, Iran.
Full-Text [PDF 4048 kb]
(731 Downloads)
| Abstract (HTML) (2207 Views)
Full-Text: (804 Views)
Introduction
Health, as one of the most important categories of social policy, has a special place in the prosperity and development of any country [1]. In recent years, extensive activities have been carried out in the countries to improve the quality of primary health care [2]. To achieve the goal of “health for all”, international organizations such as the World Health Organization (WHO) and the Organization for Economic Co-operation and Development (OECD) have presented strategies to increase the quality of services in primary health care [3]. In Iran, the family physician program in Iran was developed in 2013 for this purpose [4]. The main goal of this plan was to maintain and promote the community health and provide health services for families, regardless of age, sex, or socioeconomic status [5]. In this plan, the family physician and their group are responsible for the health of the individuals and families covered by them [6]. Many studies have been conducted to determine the strengths, weaknesses, and reasons for the failure of the family physician program in Iran. There are limited studies on the challenges of this program in Minab, Hormozgan Province, south of Iran. It is necessary to redesign and provide appropriate and localized solutions to institutionalize it in this city as much as possible. The present study aims to explore the implementation challenges of the family physician program in Minab City.
Methods
This is a qualitative study using the thematic analysis method. The participants included the health network expansion headquarters, family physician program experts, the head of the health and treatment Network, doctors and health care workers in Minab City (n=10) who were selected using a purposive sampling method until reaching data saturation. The entry criteria were willingness to participate in the study and at least five years of experience in the family physician program. Semi-structured interviews and field notes were used to collect information. The recorded interviews were transcribed and then analyzed using MAXQDA software. To determine the reliability of the data, the opinions of an external observer were used. To determine the confirmability of the data, all activities were recorded, and a report on the research process was prepared. To determine transferability, the results were discussed and cross-validated with two non-research faculty members whose positions and experiences were comparable to those of the participants.
Results
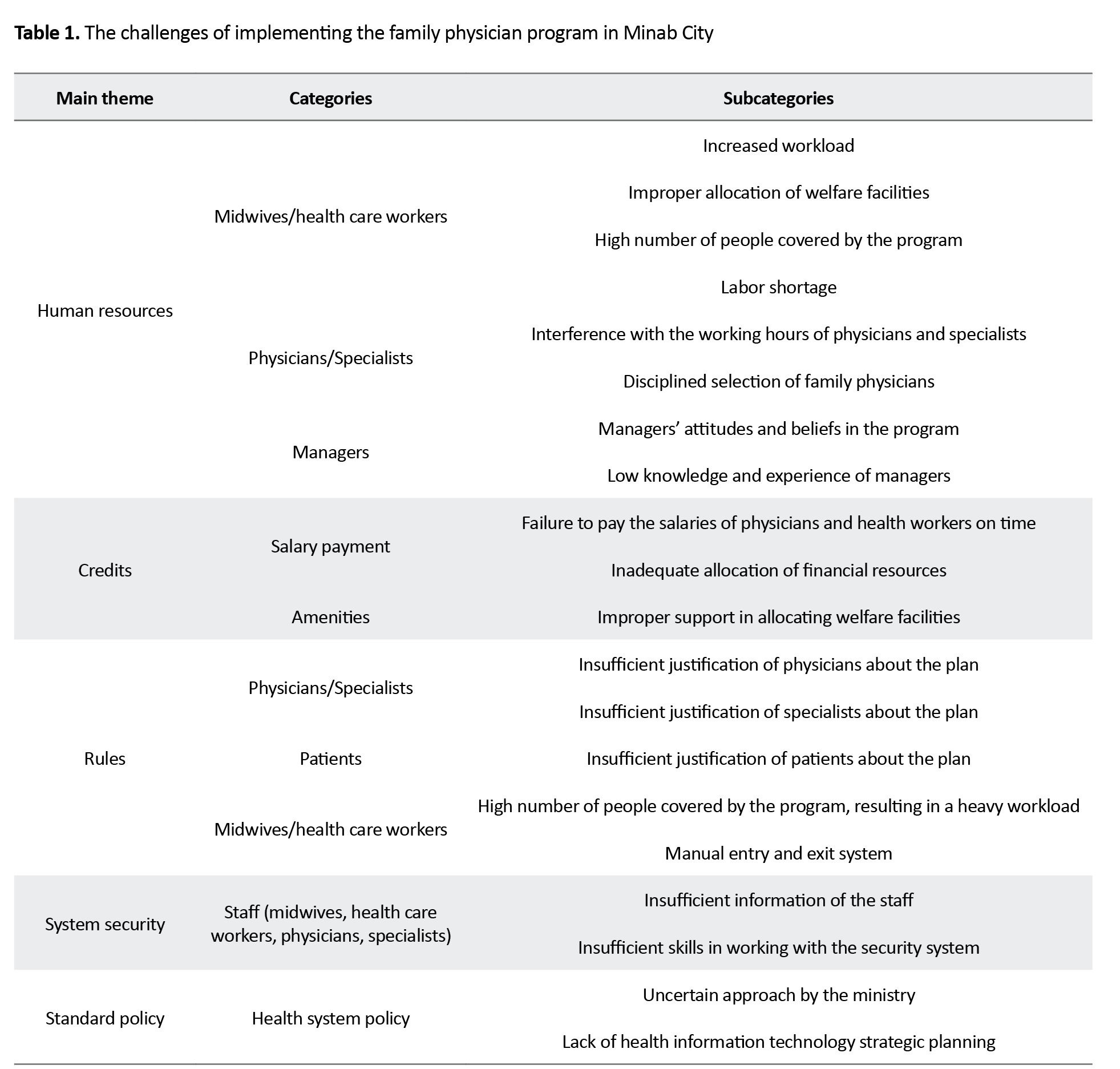
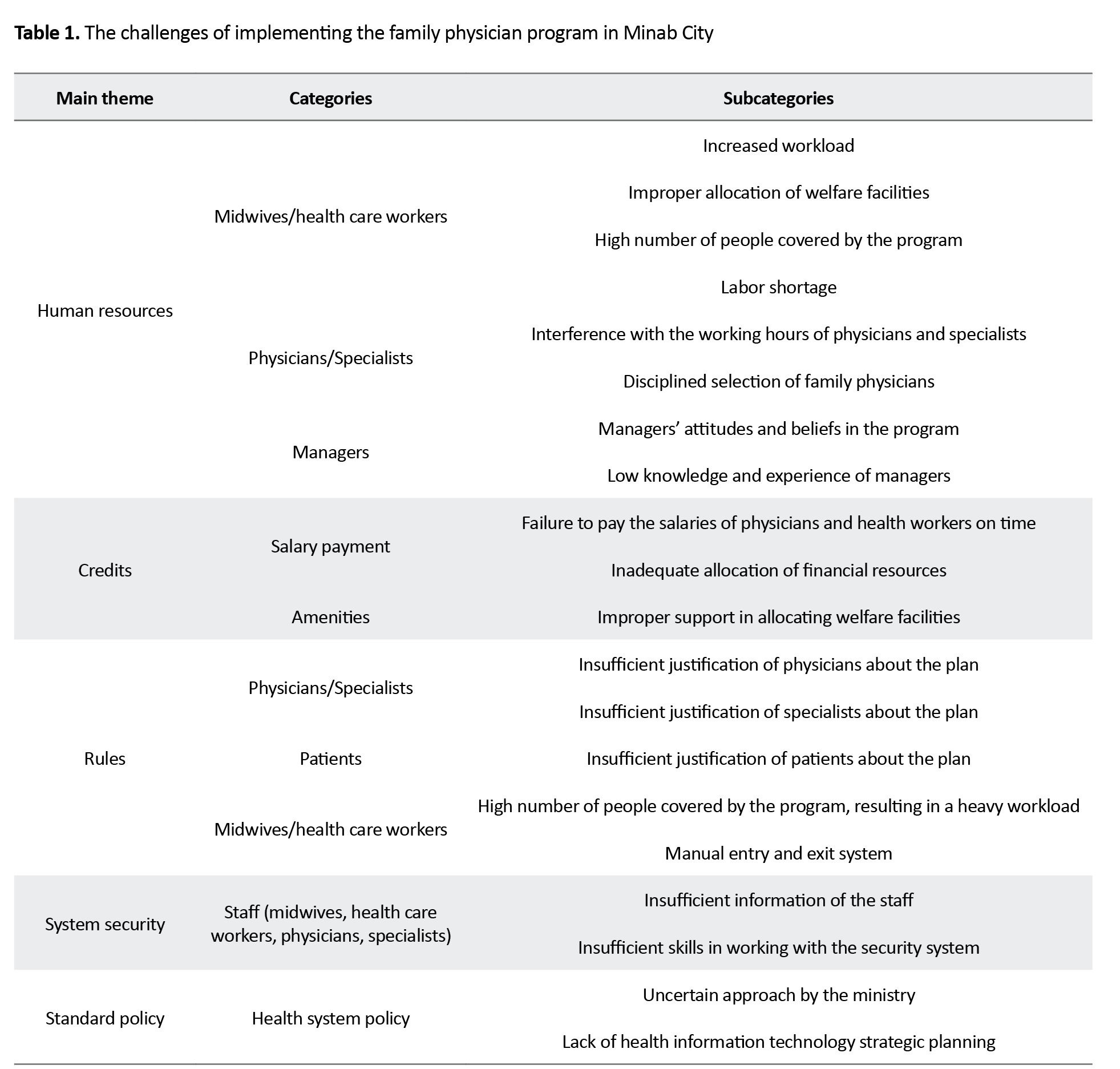
Based on data analysis, five main themes (human resources, credits, rules, system security, standard policy), 10 categories, and 20 subcategories were extracted. Table 1 shows the extracted categories and subcategories within each theme (Table 1).
Conclusion
The results of this study can lead to the adoption of policies by the Hormozgan University of Medical Sciences and the Iranian Ministry of Health and Medical Education. Also, considering that this study identified many factors related to the failure of the family physician program in Minab City, the results can be helpful in providing many educational interventions for the trustees of this plan. To solve the challenges related to implementing the family physician plan program in Minab City, it is recommended to define the manpower required for the plan, hire more health workers or reduce the population covered per physician, clarify credits in the implementation of the program, allocate more credits and sufficient funds, explain the rules in the implementation of the program, implement laws, specify disciplines for physician, health workers, and the covered population; pay attention to the security of the program implementation system, integrate the security system, justify the trustees to use the security system, define a standard model for the implementation of the program, and use the rural family physician program as a role model.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for the present research was obtained from the Ethics Committee of Marvdasht Branch, Islamic Azad University, Marvdasht, Iran (Code: IR.SUMS.REC.1402.039).
Funding
This study was taken from the master's thesis of Samireh Fakhri, approved by the Department of Health and Medical Services Management, Faculty of Humanities, Marvdasht Branch, Islamic Azad University, Marvasht, Iran.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflicts of interest
The authors declared conflicts of interest.
Acknowledgements
The authors are grateful to the Vice-Chancellor of Research, Marvdasht Branch, Islamic Azad University, Marvdasht, Iran.
References
Health, as one of the most important categories of social policy, has a special place in the prosperity and development of any country [1]. In recent years, extensive activities have been carried out in the countries to improve the quality of primary health care [2]. To achieve the goal of “health for all”, international organizations such as the World Health Organization (WHO) and the Organization for Economic Co-operation and Development (OECD) have presented strategies to increase the quality of services in primary health care [3]. In Iran, the family physician program in Iran was developed in 2013 for this purpose [4]. The main goal of this plan was to maintain and promote the community health and provide health services for families, regardless of age, sex, or socioeconomic status [5]. In this plan, the family physician and their group are responsible for the health of the individuals and families covered by them [6]. Many studies have been conducted to determine the strengths, weaknesses, and reasons for the failure of the family physician program in Iran. There are limited studies on the challenges of this program in Minab, Hormozgan Province, south of Iran. It is necessary to redesign and provide appropriate and localized solutions to institutionalize it in this city as much as possible. The present study aims to explore the implementation challenges of the family physician program in Minab City.
Methods
This is a qualitative study using the thematic analysis method. The participants included the health network expansion headquarters, family physician program experts, the head of the health and treatment Network, doctors and health care workers in Minab City (n=10) who were selected using a purposive sampling method until reaching data saturation. The entry criteria were willingness to participate in the study and at least five years of experience in the family physician program. Semi-structured interviews and field notes were used to collect information. The recorded interviews were transcribed and then analyzed using MAXQDA software. To determine the reliability of the data, the opinions of an external observer were used. To determine the confirmability of the data, all activities were recorded, and a report on the research process was prepared. To determine transferability, the results were discussed and cross-validated with two non-research faculty members whose positions and experiences were comparable to those of the participants.
Results
Based on data analysis, five main themes (human resources, credits, rules, system security, standard policy), 10 categories, and 20 subcategories were extracted. Table 1 shows the extracted categories and subcategories within each theme (Table 1).
Conclusion
The results of this study can lead to the adoption of policies by the Hormozgan University of Medical Sciences and the Iranian Ministry of Health and Medical Education. Also, considering that this study identified many factors related to the failure of the family physician program in Minab City, the results can be helpful in providing many educational interventions for the trustees of this plan. To solve the challenges related to implementing the family physician plan program in Minab City, it is recommended to define the manpower required for the plan, hire more health workers or reduce the population covered per physician, clarify credits in the implementation of the program, allocate more credits and sufficient funds, explain the rules in the implementation of the program, implement laws, specify disciplines for physician, health workers, and the covered population; pay attention to the security of the program implementation system, integrate the security system, justify the trustees to use the security system, define a standard model for the implementation of the program, and use the rural family physician program as a role model.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for the present research was obtained from the Ethics Committee of Marvdasht Branch, Islamic Azad University, Marvdasht, Iran (Code: IR.SUMS.REC.1402.039).
Funding
This study was taken from the master's thesis of Samireh Fakhri, approved by the Department of Health and Medical Services Management, Faculty of Humanities, Marvdasht Branch, Islamic Azad University, Marvasht, Iran.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflicts of interest
The authors declared conflicts of interest.
Acknowledgements
The authors are grateful to the Vice-Chancellor of Research, Marvdasht Branch, Islamic Azad University, Marvdasht, Iran.
References
- Phillips CB, Pearce CM, Hall S, Travaglia J, De Lusignan S, Love T, et al. Can clinical governance deliver quality improvement in Australian general practice and primary care? A systematic review of the evidence. Med J Aust. 2010; 193(10):602-7. [DOI:10.5694/j.1326-5377.2010.tb04071.x] [PMID]
- Baltussen R, Ye Y, Haddad S, Sauerborn RS. Perceived quality of care of primary health care services in Burkina Faso. Health Policy Plann. 2002; 17(1): 42-8. [DOI:10.1093/heapol/17.1.42]
- Roland M. Linking physicians’ pay to the quality of care-a major experiment in the United Kingdom. New Engl J Med. 2004; 351(14):1448-54. [DOI:10.1056/NEJMhpr041294]
- Berenson RA, Rich EC. US approaches to physician payment: The deconstruction of primary care. J Gen Intern Med. 2010; 25(6):613-8. [DOI:10.1007/s11606-010-1295-z]
- Perera GR, Dowell AC, Morris CJ. Constructing a framework for quality activity in primary care. Aust Health Rev. 2013; 37(1):98-103. [DOI:10.1071/AH11097]
- Abedi G, Charati JY, Marvi A. [Satisfaction of service recipients and providers in health centers with urban family physician services and other health centers in Sari and Gorgan, North of Iran (Persian)]. J Mazandaran Univ Med Sci. 2019; 29(172):80-9. [Link]
- Kabir MJ, Jafari N, Nahimi Tabihi M, Mikaniki E, Ashrafian Amir H, Nasrollahpour Shirvani SD, et al. [Health record and provided services recording among centers implementing rural family physician and insurance program in Northern provinces of Iran (Persian)]. J Hosp. 2015; 14(2):61-9. [Link]
- Omid A, Yammani N, Heidari K, Mousavi T, Mousavi A. [Educational Needs of General Practitioners Who Enrolled as Family Physicians in National Family Medicine Program and Referral System (Persian)]. Iran J Med Educ. 2013; 13(6):470-9. [Link]
- Shiani M, Rashidian A, Mohammadi A. [Status and barriers to implementation of family physician program in Iran health system (Persian)]. Soc Welfare Q. 2016; 16(62):59-102. [Link]
- Dehnavieh R, Movahed E, Rahimi H, Zareipour MA, Jadgal KM, Alizadeh S, et al. Evaluation of the referral system in Iran’s rural family physician program; A study of Jiroft University of Medical Sciences. Electronic Physician. 2017; 9(4):4225. [DOI:10.19082/4225]
- Kolesnyk P, Frese T, Vinker S, Shushman I, Zharkova A, Messaadi N, et al. Steps towards implementing evidence-based screening in family medicine in Ukraine: SWOT-analysis of an approach of multidimensional empowerment. BMC Fam Pract. 2021; 22(20):1-11. [DOI:10.1186/s12875-021-01367-2]
- Sepehri B, Ghaffari R, Jeddian A, Salek F, Emrouzi R, Ghaffarifar S, Rezvan FB. A descriptive-comparative study of implementation and performance of family physician program in iran and selected countries. Iran J Public Health. 2020; 49(3):539-48. [DOI:10.18502/ijph.v49i3.3151]
- Fardid M, Jafari M, Moghaddam AV, Ravaghi H. Challenges and strengths of implementing urban family physician program in Fars Province, Iran. J Educ Health Promot. 2019; 8(1):36. [DOI:10.4103/jehp.jehp_211_18]
- Hooshmand E, Nejatzadegan Z, Ebrahimipour H, Bakhshi M, Esmaili H, Vafaeenajar A. Rural family physician system in Iran: Key challenges from the perspective of managers and physicians, 2016. Int J Healthc Manag. 2019; 12(2):123-30. [DOI:10.1080/20479700.2017.1402422]
- Kavosi Z, Siavashi E. A study of the performance of referral system in urban family physician program in Fars Province, Iran. J Health Manag Info. 2018; 5(3):88-95. [Link]
- Leonardi F. The definition of health: Towards new perspectives. Int J Health Serv. 2018; 48(4):735-48. [PMID]
- World Health Organization. Scaling up family practice: Progressing towards universal health coverage. Geneva: World Health Organization; 2016. [Link]
- Shadmi E, Wong WC, Kinder K, Heath I, Kidd M. Primary care priorities in addressing health equity: Summary of the WONCA 2013 health equity workshop. Int J Equity Health. 2014; 13:104. [DOI:10.1186/s12939-014-0104-4] [PMID]
- European :union: of General Practitioners / Family Physicians. An opportunity to achieve sustainable Healthcare through primary care. Brussels: European :union: of General Practitioners / Family Physicians; 2022. [Link]
- Damari B, Vosough Moghaddam A, Rostami Gooran N, Kabir MJ. Evaluation of the urban family physician and referral system program in Fars and Mazandran provinces: History, achievements, challenges and solutions. J Sch Public Health Inst Public Health Res. 2016; 14(2):17-38. [Link]
- Naderimagham S, Jamshidi H, Khajavi A, Pishgar F, Ardam A, Larijani B, et al. Impact of rural family physician program on child mortality rates in Iran: A time-series study. Popul Health Metrics. 2017; 15(21):1-8. [Link]
- Mehrolhassani MH, Jahromi VK, Dehnavieh R, Iranmanesh M. Underlying factors and challenges of implementing the urban family physician program in Iran. BMC Health Serv Res. 2021; 21(1336). [Link]
- Mohammadibakhsh R, Aryankhesal A, Jafari M, Damari B. Family physician model in the health system of selected countries: A comparative study summary. J Educ Health Promot. 2020; 9(1):160. [Link]
- Shirjang A, Mahfoozpour S, Masoudi Asl I, Doshmangir L. [Challenges and strategies of implementation rural family physician in Iran: A qualitative study (Persian)]. Depiction Health. 2020; 11(1):62-73. [DOI:10.34172/doh.2020.07]
Type of Study: Orginal |
Subject:
Disaster health and health economics
Received: 2024/07/31 | Accepted: 2024/08/31 | Published: 2024/07/1
Received: 2024/07/31 | Accepted: 2024/08/31 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







 hums.ac.ir
hums.ac.ir